Breast Center
Make a New Mammogram / Breast MRI Appointment:
Call 202-741-3036
Make a New Breast Biopsy Appointment:
Call 202-741-3064

Services We Offer and Conditions We Treat:
- Biopsy
- Breast surgery
- Chemotherapy and radiation
- Navigation
- Advanced digital imaging
Breast cancer takes patients down paths they never expected. The GW Comprehensive Breast Center offers a fully integrated road map to navigate the way. Our Center provides multi-disciplinary breast care services for the early detection, diagnosis, and treatment of breast cancer using state-of-the-art technologies unavailable at any other breast center in the Metro Washington, D.C. area.
Appointments
For Mammograms / Breast MRIs: 202.741.3036
For Breast Biopsies: 202.741.3064
Combining state-of-the-art technology with superior medical and surgical care in partnership with The George Washington University Hospital, our Center has been awarded a three-year full accreditation by the National Accreditation Program for Breast Centers (NAPBC) for providing quality evaluation and management of benign and malignant breast disease.
Our Facility & Services
With an open design and spa-like interior, our Center is a comforting setting for patients to receive comprehensive breast care by our internationally recognized specialists who care only for the breast, including our all-women team of skilled breast surgeons who perform advanced surgical procedures.
As a designated Center of Excellence by the American College of Radiology for stereotactic breast therapy, breast ultrasound and ultrasound-guided biopsy, our facility provides patients with access to a full range of advanced breast imaging technology and the latest minimally invasive treatments.
Latest News
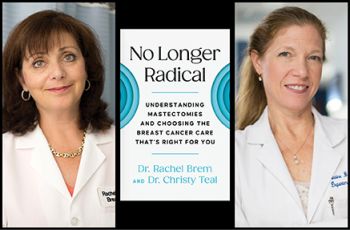
October is Breast Cancer Awareness Month, and according to the National Breast Cancer Foundation, thanks to early detection and advanced treatment the five-year survival rate for patients is 99%. Recently, Rachel Brem, MD, vice chair of radiology and director of the George Washington University…
October is Breast Cancer Awareness Month, and though the incidence of breast cancer is high, early detection is the key to successful outcomes. According to the National Cancer Society, nearly 4 million women in the United States with a history of the disease are alive today, mainly because of…